Bacterial and Fungal Infections
Bacterial Biofilms
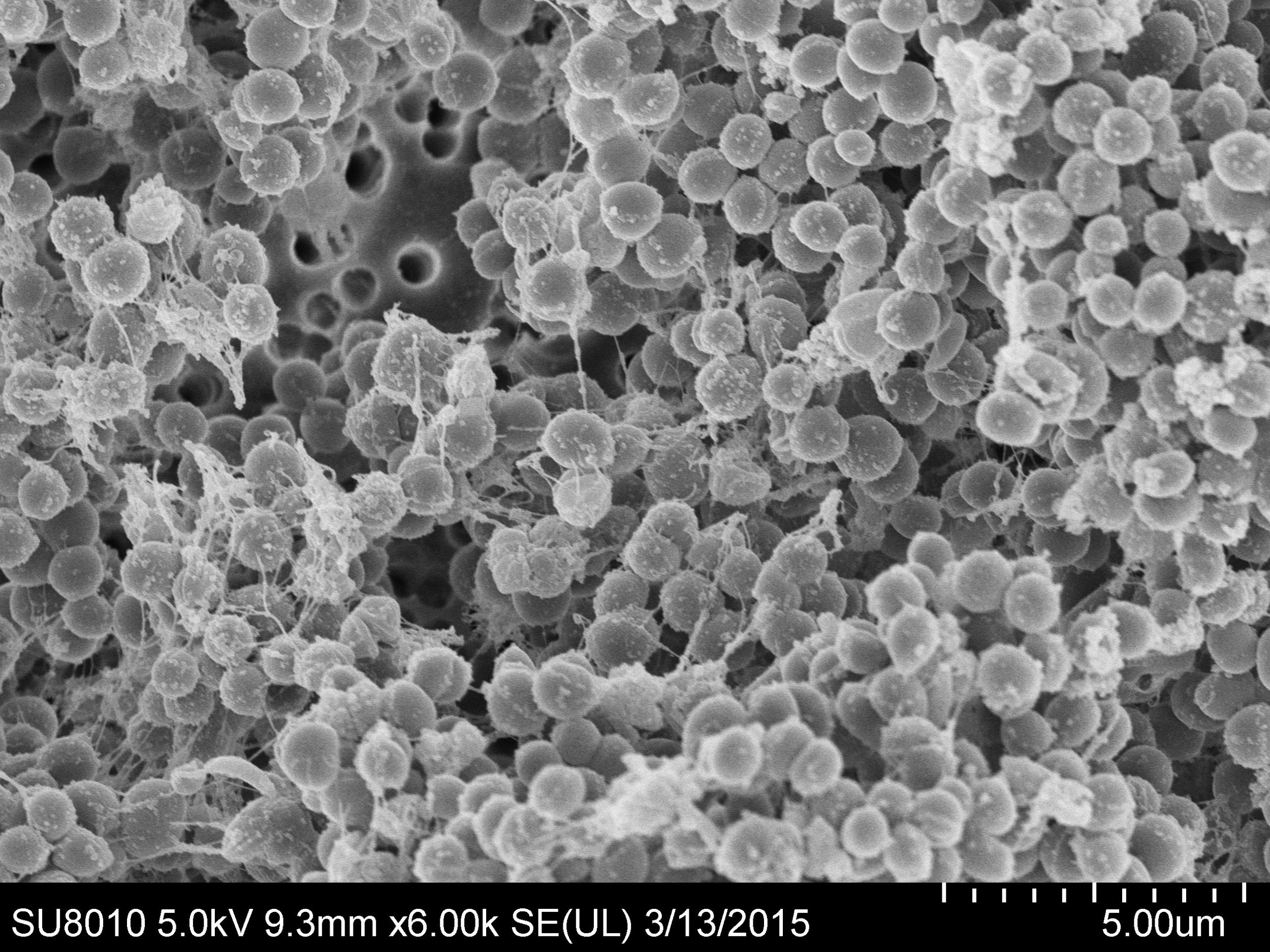
Biofilm is a non-cellular habitat for bacterial growth and is very difficult for antibiotics to penetrate. Biofilm produce various proteins and polysaccharides to form a structural barrier against intravenous and local antibiotic efficacy and immune response, where bacteria go into a resting state.
Biofilm is an important pathology in respiratory disease. It is present in the endotracheal tubes within 24 hours. There is strong experimental evidence that the organisms in the endotracheal tube biofilms go on to cause ventilator associated pneumonia. Similarly, other respiratory infections may involve biofilms such as chronic obstructive pulmonary disease, cystic fibrosis and asthma, often the cause of exacerbations. BromAc® is being developed pre-clinically for respiratory infections including those from bacteria and fungi. It rapidly dissolves biofilm established in endotracheal tubes from ventilated patients at clinically achievable doses and times (within 20 minutes of nebulising the drug). The role of BromAc® in these infections is being examined with our collaborators - it is likely to be useful in preventing exacerbations of respiratory disease and reducing the rate of biofilm associated infections in the intubated patient.
Infection of surgically implanted mesh and joint replacement sites are very serious problems that almost always require major surgery at considerable discomfort to the patient and cost to the healthcare system. Mesh implantation as part of hernia repair (inguinal, incisional) is utilised in almost 1 million patients per year in the United States alone. Approximately 1% of inguinal hernias and 8% of incisional hernias develop a serious mesh infection. Surgical mesh infections from ventral hernia repairs are common in obese patients, who are often poor surgical candidates with limited therapeutic options (including removal of the mesh). Invasive interventions precede further short- and long-term complications including the re-occurrence of infection or incisional hernias. The treatment of mesh infections with antibiotics is remarkably unsuccessful due to bacterial production of biofilm. BromAc® alone or in combination with antibiotic agents is able to break down biofilm from pseudomonas aeruginosa and staphylococcus aureus in preclinical models, improving penetration of the antibiotic to target infection. In orthopaedic and mesh infections, BromAc® is intended to be administered directly surrounding the infected cavity utilising a small radiologically placed drain. The possibility of treating infected mesh by minimally-invasive means will be attractive to both patients and health providers because of the considerably shorter hospitalisation requirements. This may be entirely performed as an outpatient.
A single nebulisation of BromAc® (5ml) reduced established biofilm in endotracheal tubes from intubated patients (mean 4.2 days in situ) by more than 85% vs. control (n=26)
Fungal Infections
Invasive fungal diseases cause substantial mortality especially in seriously ill and immunocompromised individuals. Whilst Candida and Aspergillus species are the most frequent cause of infections, opportunistic moulds, such as Mucorales are increasingly encountered with use of more intense immunosuppressive therapies. Treatment is problematic as Mucorales are intrinsically resistant to many antifungal drugs; poor prognosis for similar reasons is evident for other non-Aspergillus mould infections. Newer antifungal drug classes in late-stage clinical development lack in vitro activity against Mucorales and demonstrate little to no activity against yeasts. Mortality in COVID-19 associated Mucormycosis mirrors that in the non-COVID setting and is >50%, approaching 100% in high risk patients.
In vitro, BromAc® reduces the mean inhibitory concentrations (MIC) of the major anti-Mucorales antifungal agents up to 100-fold, as well as that for various agents (up to 100-fold) used to treat candidiasis and cryptococcosis. Interestingly, BromAc® had little effect on non-Mucorales moulds, which strengthens the importance of structure-mechanistic characteristics of both pathogen and drug.
In October 2022, the World Health Organisation released its first report on fungal "priority pathogens" – a catalogue of the 19 fungi that represent the greatest threat to public health. Despite the growing concern, fungal infections receive very little attention and resources, leading to a scarcity of quality data on fungal disease distribution and antifungal resistance patterns (with only four classes of antifungal medicines currently available and few candidates in clinical pipeline).
Mucpharm is collaborating with leading infectious diseases clinicians and government based research institutes to determine the role of BromAc® in fungal infections. The drug has been administered safely in phase 1 into the respiratory tract by nebulisation. BromAc® in combination with antifungal therapies may provide a treatment for the gaps in fungal therapies, including providing a treatment for resistant Mucorales, Candida and Cryptococcus species.
